Sometimes abnormal blood vessels grow near the optic nerve rather than underneath the fovea. The best way to treat these "peripapillary" choroidal neovascular membranes was studied by our laboratory.
Peripapillary choroidal neovascularization (PCNV) can result in significant vision loss due to extension of blood or fluid into the macula. Treatment options for PCNV have included laser photocoagulation, subretinal surgery and photodynamic therapy. More recently, intravitreal anti-VEGF antibodies has emerged as the optimal treatment for macular CNV due to AMD, POHS, myopia, angioid streaks, and traumatic choroidal rupture, but clinical trials contained, almost exclusively, patients with subfoveal choroidal neovascularization. The purpose of this study was to review cases of PCNV treated with intravitreal bevacizumab.
Published in the journal Archives of Opthalmology, we found that 17 of 20 eyes (85%) achieved resolution of the fluid after an average of 2.4 intravitreal injections of bevacizumab, and five of these had recurrent fluid. Visual acuities improved by an average of 5 letters or one line of Snellen acuity after an average of 13.5 months of follow up, and only one patient lost vision limited to one line.
Overall, it is our impression that PCNV responds to intravitreal bevacizumab with reduction of retinal fluid and improvement or preservation of vision comparable to other treatment modalities. PCNV cases of recurrent or incomplete fluid resolution, intravitreal bevacizumab may still shrink lesions prior to other treatment. Further prospective and comparative studies are required to better understand the risks, benefits and limits of this therapeutic modality.
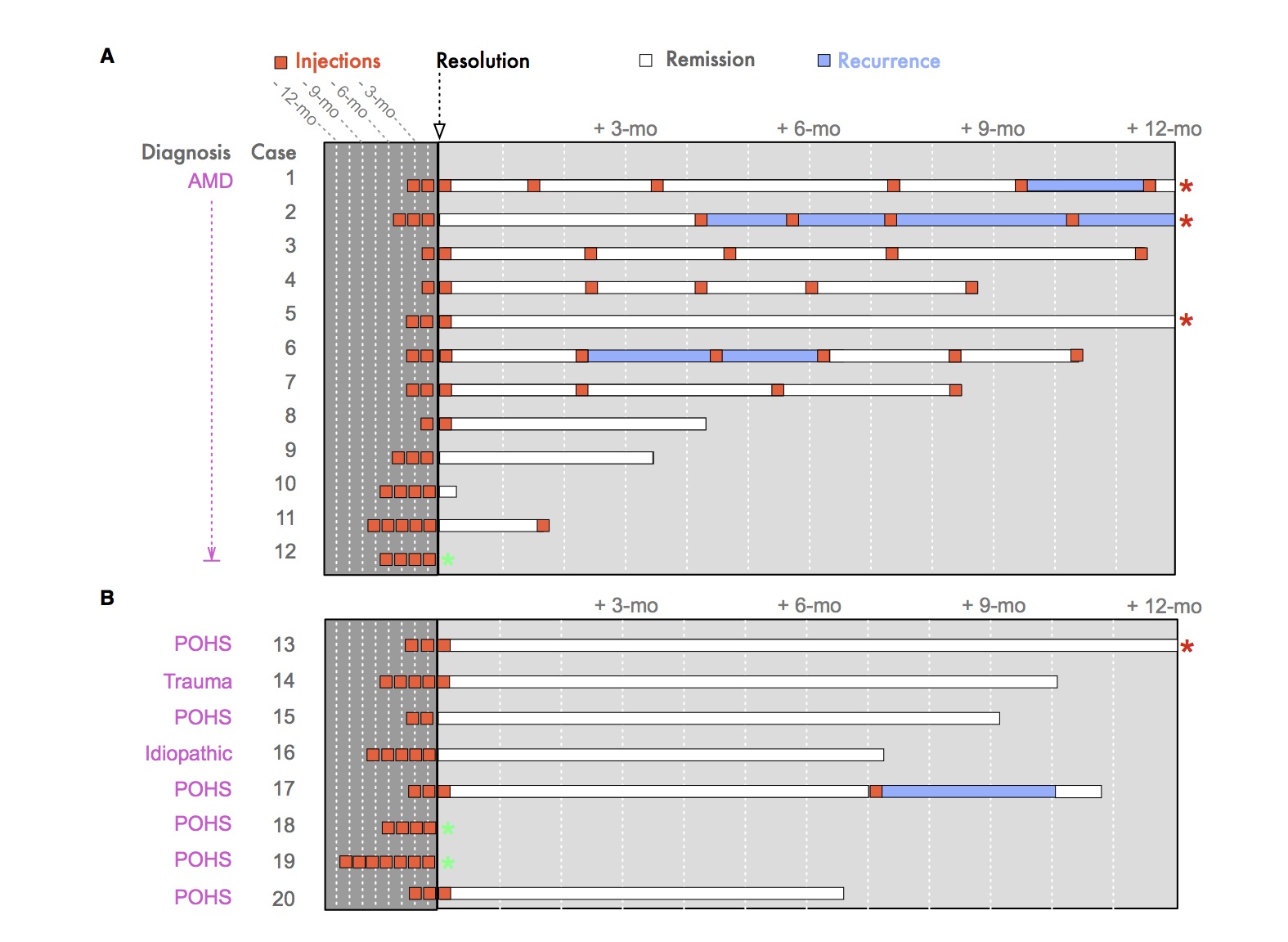
To better understand how patients respond to intravitreal injections, we designed a new infographic to illustrate the complex treatment pattern and patient responses. In the figure below, the timeline shows treatment and response to intravitreal bevacizumab in 20 eyes with peripapillary choroidal neovascularization (PCNV). A, PCNV was diagnosed in 12 eyes with age-related macular degeneration (AMD). B, PCNV was diagnosed in 8 non-AMD eyes, presumed ocular histoplasmosis (POHS) (6/8), trauma (1/8) and idiopathic cause (1/8). Resolution of fluid is indicated by the black arrow. The number of injections (orange boxes) given at 4-6 week intervals that were required to achieve resolution of fluid on OCT are shown to the left (dark grey box). The number of injections following resolution of fluid is shown to the right (light grey box). Periods of fluid remission (white rectangles). Periods of recurrent fluid (blue rectangles). Follow-up time is indicated on the x-axis. Four patients had greater than 12-months of follow-up (orange asterisk). Three patients did not achieve fluid resolution at their last follow-up visit (green asterisk).