ADNIV is an inherited autoimmune disease of the eye. We performed a study to determine the benefit of Retisert, an implant that delivers steroids within the eye for several years.
In a study published in the journal, Archives of Ophthalmology, we found that the implant inhibited specific features of ADNIV such as inflammatory cells and neovascularization. Additional therapies are needed to stabilize long-term vision, retinal thickening, and fibrosis.
Nine eyes of five related ADNIV patients with uncontrolled inflammation were reviewed. Follow-up ranged 21.7–56.7 months. Vision at implantation ranged from 20/40 to hand motion. Preoperatively, eight eyes demonstrated vitreous cells (an eighth had a diffuse vitreous hemorrhage). Eight eyes demonstrated cystoid macular edema, seven had an epiretinal membrane, and three manifested retinal neovascularization. Following implantation, vitreous cells resolved in all eyes and neovascularization regressed or failed to develop. Central macular thickness improved in four eyes. During the postoperative course, however, visual acuity continued to deteriorate, with vision at the most recent examination ranging from 20/60 to no light perception. There was also progressive intraocular fibrosis and phthisis in one case. Four eyes underwent cataract surgery. Six of the seven eyes without previous glaucoma surgery demonstrated elevated intraocular pressure at some point, and three of these required glaucoma surgery.
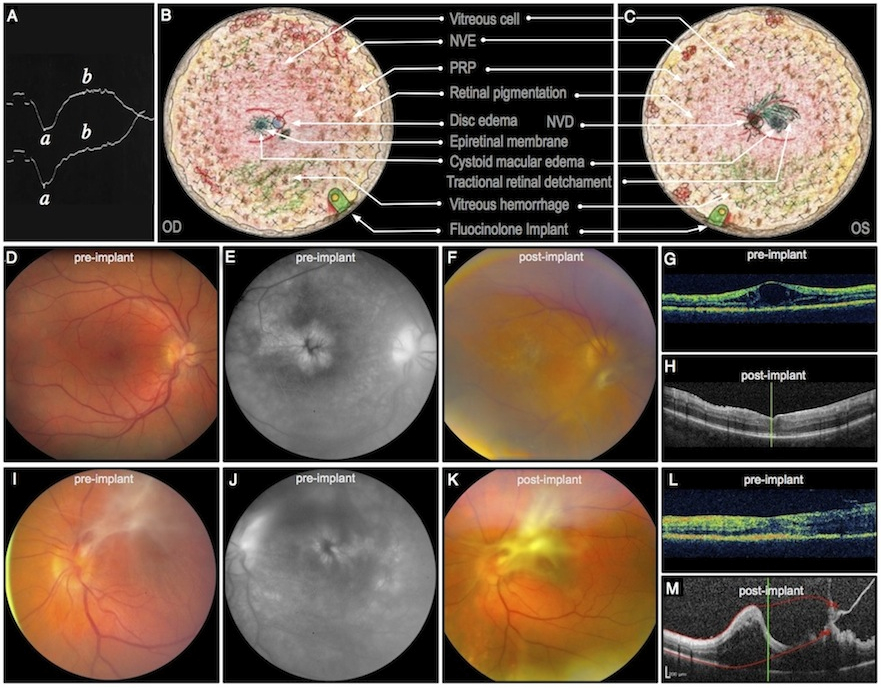
A case of ADNIV is presented in the figure below. A. An electroretinogram showing a diminished b-wave helped diagnose patient 1 with ADNIV at age 17. B, C. Composite fundus drawings show vitreoretinal pathology overlaid with treatment that took place over several years beginning at age 21 when his visual acuity was 20/100 OU. He developed aggressive ADNIV with cystoid macular edema, an epiretinal membrane, and small punctuate areas of peripheral neovascularization and vitreous hemorrhage OD. There was a central vitreous hemorrhage secondary to neovascularization of the disc with count fingers vision OS. Traction was noted in the periphery OS. Both eyes showed characteristic peripheral pigmentary changes. Oral steroids and panretinal scatter photocoagulation initially stabilized the patient to 20/30 OD and 20/50 OS. He subsequently lost vision due to continuous inflammation, CME, and recurrent vitreous hemorrhage while on steroid-sparing agents over the next two years, including methotrexate and infliximab, and moderate doses of prednisone. At age 24, fluocinolone acetonide implants were placed in each eye. D. Preoperative fundus image OD shows an epiretinal membrane and CME (VA 20/100). E. CME was confirmed by fluorescein angiography. F. Postoperative fundus image shows worsening membrane OD. G, H. Pre and postoperative OCT shows CME that resolved soon after device implantation. Within one month after surgery, a mild CRVO developed, and the patient was treated with oral steroids. A small area of retinal neovascularization was noted at that time, precipitating a dose of intravitreal bevacizumab and further laser photocoagulation. All vascular changes regressed in six months. Cataract surgery and trabeculectomy OD were performed one and two years after implant placement, respectively. The right eye also required a laser peripheral iridotomy for pupillary block, but inflammation was controlled nearly four years after device implantation without need for replacement. I. Preoperative fundus image OS shows regressed NVD, preretinal fibrosis, and epiretinal membrane. J. Findings consistent with recurrent CME are apparent on preoperative fluorescein angiography. K. Postoperative fundus image shows progressive fibrosis OS. L. The immediate preoperative OCT shows early tractional membranes superiorly (right side of OCT), without traction on the fovea or significant CME. M. Postoperative OCT shows increased tractional membranes. Implantation OS was followed nearly immediately by elevated intraocular pressure that was controlled initially with topical glaucoma medication. Initially, the vision OS stabilized to 20/60 without recurrent CME, neovascularization, or hemorrhage. One year later, cataract surgery was performed, and two years later the implant was replaced and a trabeculectomy was performed. The only systemic immunomodulatory medications this patient received at any time after initial implant surgeries were short courses of prednisone for a mild central retinal vein occlusion OD and any subsequent intraocular surgeries. Despite control of neovascularization and vitreous cell, there was worsening of preretinal fibrosis and tractional membranes and deterioration of visual acuity to 20/80 OD and 20/200 OS. (ADNIV, autosomal dominant neovascular inflammatory vitreoretinopathy; CME, cystoid macular edema; CRVO, central retinal vein occlusion; NVD, neovascularization of the disc; OCT, optical coherence tomography; OD, right eye; OS left eye; VA, visual acuity.)